FRONTIERS IN MEDICAL CASE REPORTS - Volume 6; Issue 4, (Jul-Aug, 2025)
Pages: 01-07
Print Article
Download XML Download PDF
A Case of Central Retinal Arterial Occlusion following Arthroscopic Shoulder Surgery
Author: Hassan Abou Adma, Huy Tran, Martin Holguin, Daniel Romanelli
Category: Medical Case Reports
Abstract:
Postoperative visual loss (POVL) is a rare but serious complication that can occur after non-ocular surgery, with a limited number of documented cases in arthroscopic procedures. The main causes of POVL are central retinal artery occlusion (CRAO), ischemic optic neuropathy (ION) and cerebral vision loss with multiple risk factors. This case report highlights a patient who developed POVL after arthroscopic shoulder surgery, shedding light on possible mechanisms and contributing factors.
A 52-year-old man with chronic shoulder pain underwent arthroscopic shoulder surgery. The patient had mild hypertension, a smoking history and slightly elevated lipid levels. After surgery, he developed a sudden loss of vision in his right eye, which led to extensive evaluation. Various tests ruled out stroke, heart problems and other causes. The patient was discharged with eye medication and his vision improved significantly within two weeks.
POVL after non-ocular surgery is an important but poorly understood complication. Common causes include ION, CRAO, and others. The incidence is higher with spinal surgery, and anesthesia and positioning increase the risk. This case emphasizes the importance of vigilance and prevention. In this case, the most likely cause was non-arterial CRAO, possibly due to embolism, given the patient's risk factors. The exact position of the patient probably did not play a role. An interscalene block (ISB) was used, but the risk of POVL associated with ISB was low.
Although POVL is rare in arthroscopic surgery, careful consideration of various factors, including patient risk factors, surgical techniques, and positioning is critical to prevent this devastating complication.
Ensuring accurate ISB injection, regular head and neck checks, and adequate eye padding can minimize the risk. Evaluation of other possible causes, such as CRAO and ION, should lead to the necessary tests and interventions to reduce progression and future risks.
Keywords: Modified Beach Chair Position, Head Positioning, Interscalene Block, Central Retinal Artery Occlusion (CRAO), Arthroscopic Shoulder Surgery, Postoperative Vision Loss (POVL)
Full Text:
Introduction
Postoperative vision loss (POVL) is a rare yet devastating complication that can occur in various non- ocular surgeries. It is especially rare in patients undergoing arthroscopic surgeries, with a handful of cases documented (Bhatti and Enneking, 2003; Lee et al., 2016). The major causes of POVL are central retinal artery occlusion (CRAO), ischemic optic neuropathy (ION), and cerebral vision loss (Newman et al., 2008), with risk factors ranging from advanced age, hypertension, smoking, diabetes, hyperlipidemia, prone positioning, and hypotension (Calway et al., 2018).
This case highlights a patient developing POVL following arthroscopic shoulder surgery. The report provides insight into potential mechanisms and raises important observations into various factors that can lead to the progression of this dreaded complication.
Case Presentation
The patient is a 52-year-old male who initially presented with right chronic shoulder pain for the past ten years. Diagnostic imaging, including X-ray and MRI, confirmed mild to moderate supraspinatus tendinosis, delamination of the subscapularis tendon, joint effusion, and acromioclavicular arthrosis. The patient failed conservative measures with a previous steroid injection and 5 weeks of physical therapy, after which he agreed to arthroscopic shoulder surgery. His medical history includes mild hypertension (130/90 mmHg), diagnosed 2 weeks prior to surgery by his primary care provider, and was started on losartan 25mg daily. His past surgical history includes a hemorrhoid removal procedure. Family history includes the patient's father, who has hypertension and experienced a stroke in his 60's. The patient took celecoxib as needed for pain control and is allergic to penicillin. He is a former smoker who quit 30 years ago, admits to drinking alcohol socially, and denies illicit drug use. The patient is of average build, with a height of 165.1 cm, weighing 85 kg, and a BMI of 30.45. The patient also gets checkups with labs every 6 months from his primary care provider. The patient reported having typical lab values besides slightly elevated lipids at checkups.
In the preoperative setting, the anesthesiologist administered the interscalene block (ISB) and the standard induction, oral endotracheal intubation, and prophylactic IV antibiotics without incident. He was placed in a modified beach chair position. The head and torso were at approximately a 60-70 degree position with adequate padding of all bony prominences and bilateral safety straps applied, securing the patient in position; the patient's head was slightly turned to the left without placing any tension on the neck and put on a brown head gel holder with silk tape used to wrap the patient's head securing him to the chair head positioner. After the patient was securely strapped down to the beach chair, the operative arm was properly cleaned by the circulating OR nurse using Chloraprep skin prep solution. Patient was sterilely draped and 10 pounds of traction was used on the arm pulley system to allow for increased joint space during arthroscopic procedure.
A diagnostic shoulder arthroscopy was performed using standard technique, revealing a partial intra articular torn subscapularis, complex full-thickness supraspinatus tear, and gross bicep tenosynovitis. Due to the nature of the complex pattern, marginal convergent sutures were utilized along with a double row technique rotator cuff repair, an intra articular loop ‘n’ tack subscapularis, and a bicep tenodesis procedures were performed. Additionally, operations on a subacromial decompression acromioplasty were performed due to the chronic Impingement. The surgery lasted approximately two hours, and no reportable issues were noted.
After recovering from the effects of anesthesia in the postoperative setting, the patient reported that he could not see out of his right eye. Initial physical and neurological exams revealed significant vision loss. Otherwise, normal findings were noted, such as no facial drooping and regular limb movements. He denied experiencing any chest pains, shortness of breath, or headaches. Vitals taken throughout the hospital stay included blood pressure ranges from 92/54 to 157/91 mmHg, heart rate ranges from 67 to 114 BPM, and temperature, respiratory rates, and oxygen saturations were otherwise within normal limits. Labs were ordered, including general chemistry, general coagulation, general hematology, lipids, sedimentation rate, A1C, and troponin. The abnormal lab findings included A1C = 6.2%, triglycerides = 232 mg/dL (other lipids were normal), and WBC was 13.40 x 10^3/mcL, which was expected after surgery. All other lab values were within normal limits.
CT and MRA head scans ruled out cerebral vascular accidents, trans-esophageal echo scans revealed normal heart and vessels, and carotid doppler scans were within normal limits. Ophthalmological exams also revealed monocular vision loss, but no causes were determined. The patient was cleared for discharge home in stable condition the following day since all imaging and labs were insignificant. He was discharged home with tramadol and ophthalmic medications, including latanoprost, dorzolamide- timolol, brimonidine, and acetazolamide.
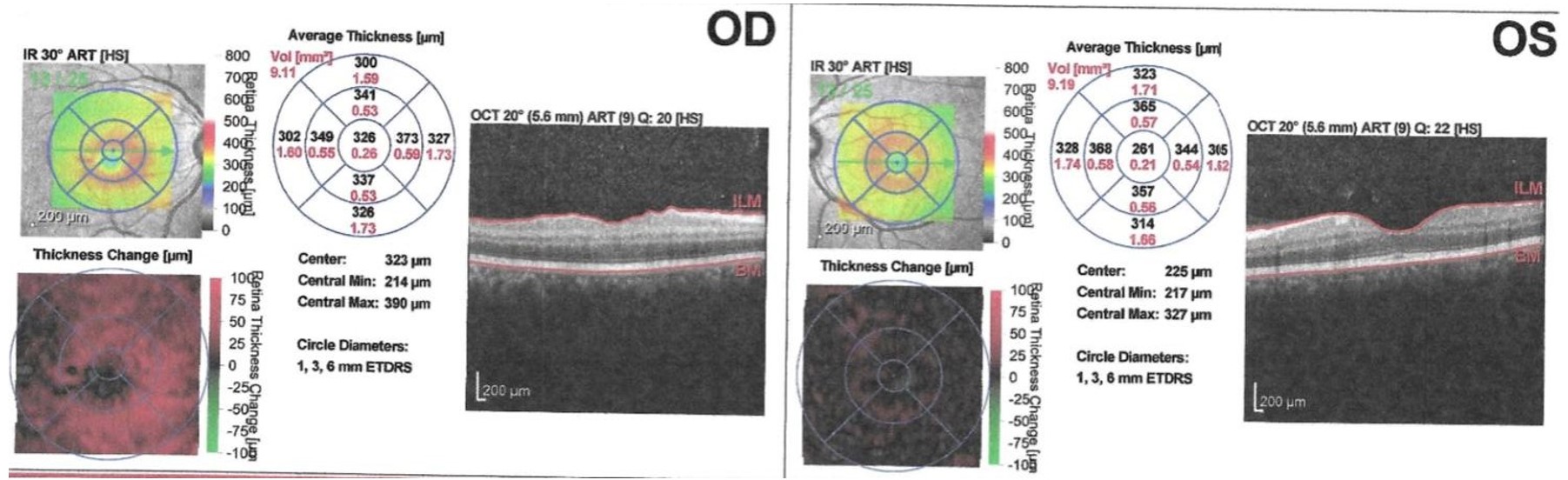
After 48 hours, the patient experienced some improvement in vision out of the right eye, reporting seeing dark shapes and shadow-like figures. On the second day following discharge from the hospital, he visited the ophthalmologist as an outpatient. The ophthalmologist conducted a dilated fundus exam and an optical coherence tomography revealing a central retinal thickness of 326 microns, Fig. 1, consistent with central retinal artery occlusion. The subsequent follow ups with the ophthalmologist confirmed total ocular circulation. Within two weeks, the patient reported a near resolution of his right eye with 20/20 vision.
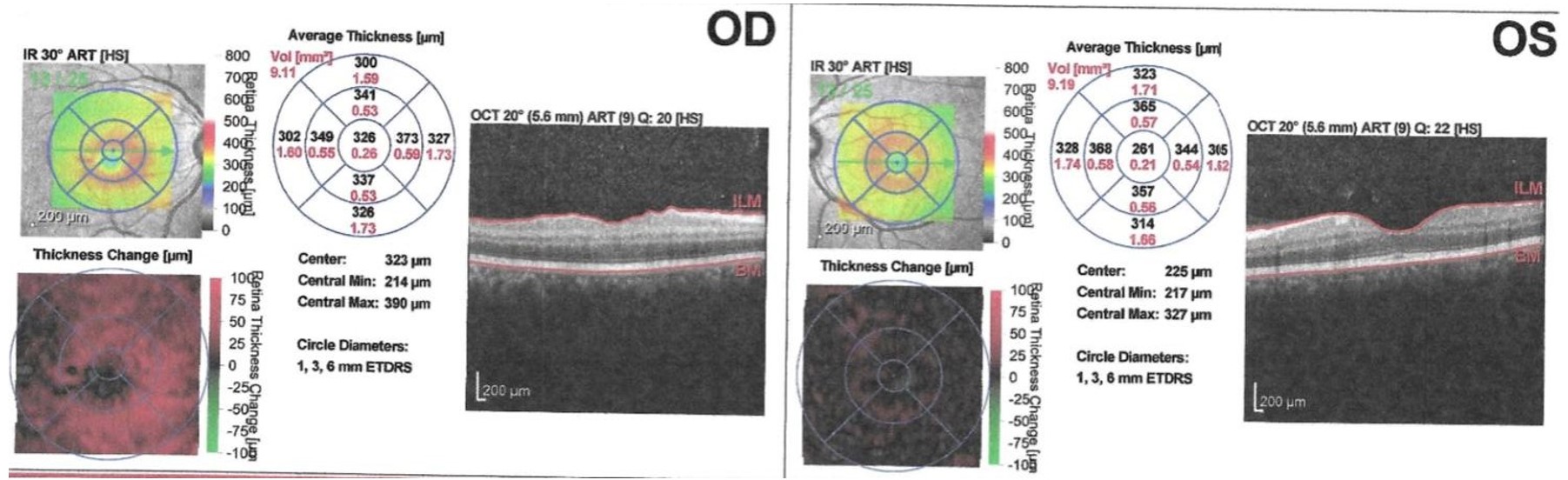
Figure 1: Retinal Optical Coherence Tomography (OCT) showing CRAO on OD compared to OS.
Discussion
In this report, we highlight a rare presentation of postoperative vision loss that developed shortly after the patient recovered from the effects of anesthesia. POVL following non-ocular surgery is a serious complication where the causes are not fully understood. The most common causes of POVL include Ischemic Optic Neuropathy (ION), Central or Branch Retinal Artery Occlusion, cortical blindness, external ocular injuries, and acute glaucoma (Mendel et al., 2017; Grover and Jangra, 2012). Although not directly linked to surgery, macular edema can cause blurry or wavy vision [1].
The epidemiology of POVL reveals that its incidence following spine surgeries exceeds that after cardiothoracic surgeries, with estimates ranging from 0.028% to 0.2%. In a study of 93 cases of visual loss after spine surgery, ION was the cause in 83 (89%) of these cases. Anesthesia itself can contribute to vision loss, particularly in the context of spine and cardiac surgeries. Residual effects of anesthetic agents may mask the initial signs and symptoms of visual loss in the postoperative period. The American Society of Anesthesiologists (ASA) has reported on cases of visual loss after spine surgery, with ION being a common cause (Mendel et al., 2017; Grover and Jangra, 2012).
Another similar case report highlights the rare complication of POVL in orthopedic surgery, specifically after reverse shoulder arthroplasty (Mumith and Scadden, 2014). Fortunately, the patient in that case fully recovered at 10 months postoperatively. The etiology of POVL is challenging to elucidate due to its elusive nature, and there are no known curative treatment options. The report emphasizes the importance of vigilance and preventative measures to avoid this devastating complication.
As for this case, we believe the most likely cause for the patient’s POVL is central retinal artery occlusion (CRAO), specifically non-arteritic CRAO caused by a transient thromboembolic event which reigns as the most common cause (Varma et al., 2013; Farris and Waymack, 2023). His history of hypertension and smoking increases his risks of developing atherosclerotic plaques leading to emboli formation. Our patient also has a family history of hypertension and stroke. The patient’s hospital labs showed an elevated A1c of 6.2%, suggesting a prediabetic state. Diabetes increases the risk of CRAO through the risk of developing atherosclerosis, thromboembolic events, and microvascular damage in the retinal circulation. Non-arteritic CRAO accounts for 15-17% of total CRAOs with the best prognosis compared to other subtypes (Varma et al., 2013). It is logical to assume this diagnosis is due to the patient’s gradual vision regain in addition to the circulation within the arterial system of the eye to be within normal limits, suggesting the resolution of the emboli.
Patient positioning is another cause of POVL to consider as it is one of the common causes due to external compression of the eye leading to increases in intraocular pressure impeding the flow in the central retinal artery (Grover and Jangra, 2012). Most commonly seen in procedures in which the patient is in a prone position, mainly during spine surgeries, external pressures can be elicited on the eyes, hence why constant reevaluation of the patient is necessary to prevent the development of POVL (Grover and Jangra, 2012; Murphy et al., 2019). However, this is an unlikely scenario due to our patient being in a modified beach chair position with adequate head positioning free of any tension in the head and neck region and constant reevaluation of the patient to ensure no external compression of the eyes was noticed. The modified beach chair position is often recommended over the traditional beach chair position, although direct comparisons in the literature are limited. The traditional beach chair position has been associated with reductions in regional brain oxygenation, cerebral blood flow, jugular bulb oxygenation, and impairment in cerebral autoregulation (Murphy et al., 2019). Therefore, it is reasonable to consider that the modified position may offer advantages in reducing the risk of cerebral desaturation events, which have been associated with the development of POVL. The head and torso of our patient were at approximately a 60-70 degree position. However, with any orientation the body is placed in, the head and neck orientation should be adjusted preoperatively and periodically checked (<= every 30 minutes) for lack of pressure on the eyes, nose, and ears (Murphy et al., 2019). Clearing the head and neck from any extreme ROMs exerting large forces on the neck can decrease the risk of obstruction of CSF flow, vertebral or carotid artery obstruction, and cerebral infarction (Murphy et al., 2019).
An ISB was used on this patient in addition to anesthesia induction plus IV antibiotics prior to surgery, which could be a risk factor in developing POVL. ISB is one of the most reliable techniques for upper extremity procedures (Carden and Ori, 2005), most commonly shoulder surgeries. POVL as a cause of ISB is unlikely to occur in this patient due to carotid scans being within normal limits. A meta-analysis of 16 studies, including 577 receiving ISB looked into safety outcomes; the study reported major complications occurred including postoperative dyspnea, pneumothorax, Horner’s syndrome, recurrent laryngeal nerve palsy, and ipsilateral paresthesia, weakness, tingling (Hussain et al., 2017). However, it can be considered a risk due to the needle’s close proximity to the carotid artery and vertebral artery, which can lead to puncture and vasospasm of the artery (Mumith and Scadden, 2014; Carden and Ori, 2005; Zisquit and Nedeff, 2018).
Conclusions
Although POVL is a rare complication following arthroscopic surgeries, it is important to consider various factors and precautions before surgery to ensure patient safety.
By looking at controllable factors within surgery, a decrease in complication risk is achievable, considering surrounding structures and bony landmarks to acquire accurate ISB injection so as not to lead to direct puncture of an artery within close proximity. As well as reevaluating the patient head and neck positioning every 30 minutes or less and providing sufficient padding of the eyes not to allow increases in IOP, or prolonged hypotensive episodes leading to progression of POVL. When considering other causes of POVL, such as CRAO and ION, this can prompt the evaluation team to request necessary tests and interventions to limit its progression and minimize risks of future incidences.
Consent: Obtained.
References:
Bhatti MT, Enneking FK. Visual loss and ophthalmoplegia after shoulder surgery. Anesth Analg 2003; 96: 899-902.
Calway T, Rubin DS, Moss HE, Joslin CE, Mehta AI, Roth S. Perioperative Retinal Artery Occlusion: Incidence and Risk Factors in Spinal Fusion Surgery from the US National Inpatient Sample 1998-2013. J Neuroophthalmol 2018; 38: 36-41.
Carden E, Ori A. Applying cervical spine anatomy to interscalene brachial plexus blocks. Pain Physician 2005; 8: 357-361.
Farris W, Waymack J. “Central retinal artery occlusion”, National Center for Biotechnology Information. 2023.
Grover V, Jangra K. Perioperative vision loss: A complication to watch out. J Anaesthesiol Clin Pharmacol 2012; 28: 11-16.
Hussain N, Goldar G, Ragina N, Banfield L, Laffey JG, Abdallah FW. Suprascapular and Interscalene Nerve Block for Shoulder Surgery: A Systematic Review and Meta-analysis. Anesthesiology 2017; 127: 998-1013.
Lee J, Chin JH, Koh WU, Ro YJ, Yang HS. Unilateral postoperative visual loss in a patient undergoing hip arthroscopy in the supine position: a case report. Korean J Anesthesiol 2016; 69: 197-199.
Mendel E, Stoicea N, Rao R, Niermeyer W, Revilla S, Cluse M, Sandhu G, Todaro GJ, Bergese SD. Revisiting Postoperative Vision Loss following Non-Ocular Surgery: A Short Review of Etiology and Legal Considerations. Front Surg 2017; 4: 34.
Mumith A, Scadden J. Postoperative vision loss after reverse shoulder arthroplasty. Case Rep Orthop 2014; 2014: 850950.
Murphy GS, Greenberg SB, Szokol JW. Safety of Beach Chair Position Shoulder Surgery: A Review of the Current Literature. Anesth Analg 2019; 129: 101-118.
Newman NJ. Perioperative visual loss after nonocular surgeries. Am J Ophthalmol 2008; 145: 604-610.
Varma DD, Cugati S, Lee AW, Chen CS. A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond) 2013; 27: 688-697.
Zisquit J, Nedeff N. Interscalene Block, National Center for Biotechnology Information (2018).
Links
1. Macular Edema | National Eye Institute. https://www.nei.nih.gov/learn-about-eye-health/eye- conditions-and-diseases/macular-edema.
|